TECHNICAL ASSISTANCE: BECOME A RURAL TRAINING SITE START A RURAL PROGRAM
Start a Rural GME Program
Getting Started with Program Development:
To set up an initial discussion about the possibilities for developing a rural training program at your Wisconsin residency program, contact WCRGME. Please refer to the resources below as you begin this journey to establish graduate medical education (GME).
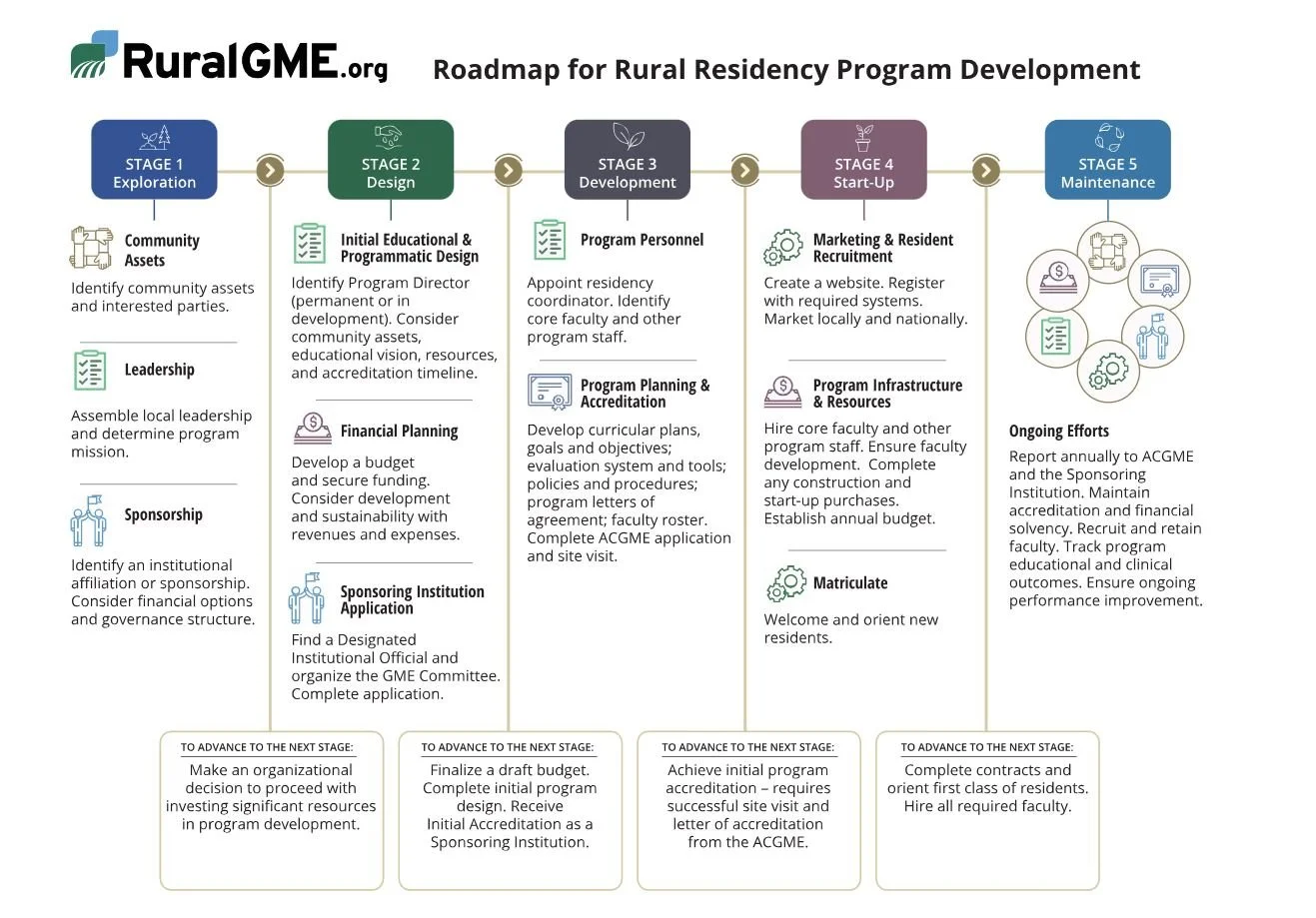
“Roadmap for Rural Residency Program Development” model outlined in the figure below details the progressive stages of the process, from early interest and recognized need for a GME program to meet local health care needs, to the implementation of a functional, accredited, and financially sustainable program. Additional resources and tools for developing rural residencies are available at ruralgme.org.
About Rural Residencies
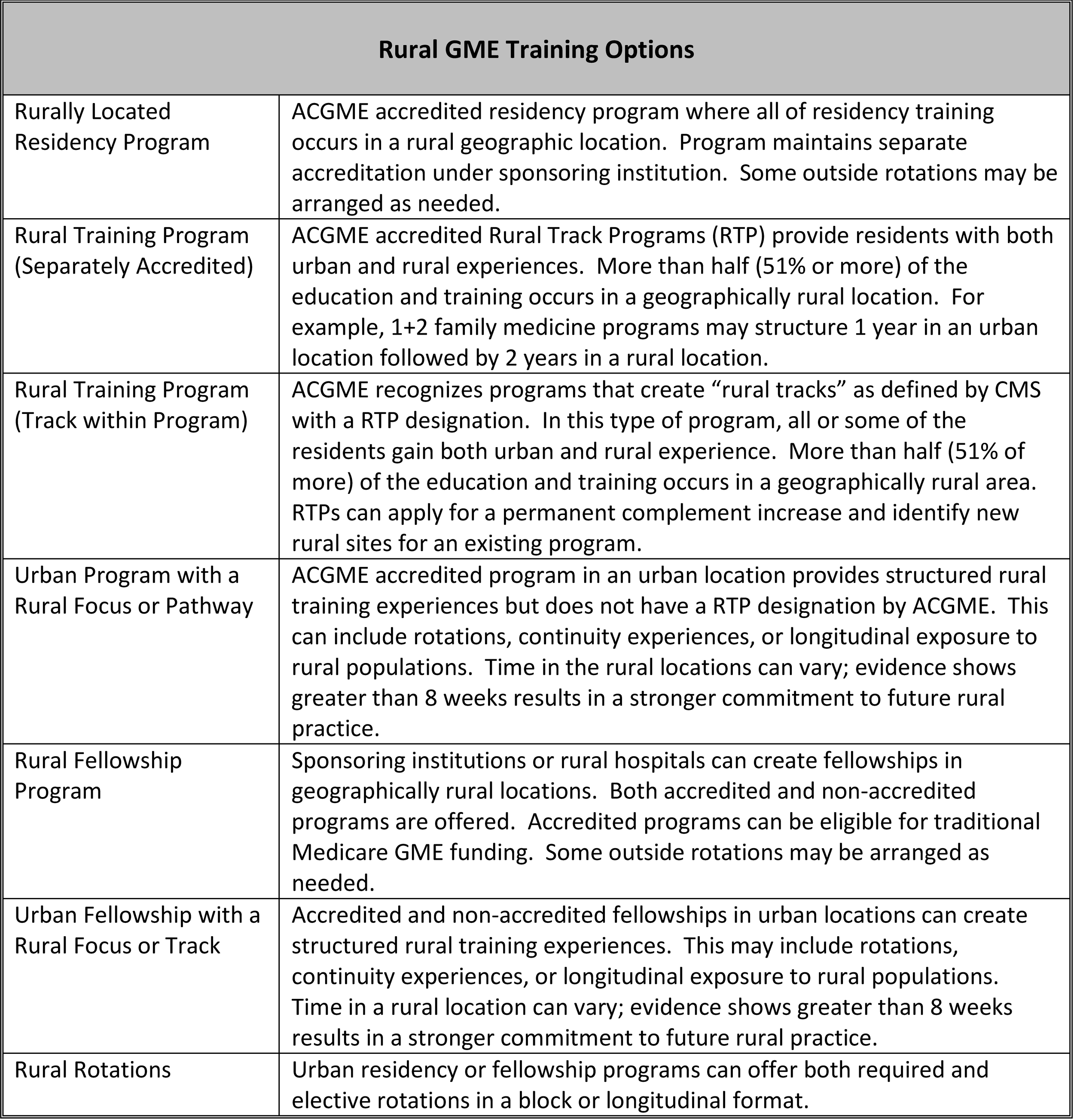
A rural residency program is an accredited graduate medical education program in which trainees spend a majority of their time (more than 50%) in a rural place. Programs can be rurally located, structured to provide a combination of rural and urban experiences (Rural Training Programs or RTPs), or may exist as an expansion of an urban program.
Rural residencies are a critical tool in recruiting and retaining physicians to rural Wisconsin. Evidence shows that “…medical residents who train in rural settings are two to three times more likely to practice in a rural area; especially those who participate in a rural training track.”
(Patterson DG, Longenecker R, Schmitz D, Skillman SM, Doescher MP. Policy Brief: training physicians for rural practice: capitalizing on local expertise to strengthen rural primary care. Collaboration of Rural Training Track Assistance Program and WWAMI Rural Health Research Center; 2011)
Benefits of Rural Training:
Reduced recruiting costs (estimated at $100,000 per primary care physician)
Enhanced recruitment of faculty and specialty physicians who wish to teach
Improved retention of faculty and specialty physicians who wish to teach (replacement costs for a primary care physician is estimated at $250,000 or more, and is generally greater for sub-specialty physicians)
“Contribution margin” and downstream revenue to hospitals (although difficult to quantify directly, many hospitals use this calculation in budgeting)
Leadership development of existing medical staff
Improved quality of care (Direct involvement of faculty and residents in quality efforts, indirect effect of a learning culture)
Reputation as a teaching hospital
Increased primary care clinical capacity and community access to care
Other health professions education and training (a graduate medical education infrastructure becomes the framework for an interprofessional campus of learners)
Economic benefit to the community (Every faculty physician or resident recruited or retained has been shown to lead to $1-2 million in economic benefit to the community annually, particularly for those family physicians who practice obstetrics)
Community leadership by physicians and their families (many physicians wear hats in their community outside medicine)
Civic engagement by both faculty and residents and their families
Creativity and innovation
(Planting TREES in Rural Places Training and Rural health professions Education that is community Engaged and Sustainable January 2019 Randall Longenecker MD, Executive Director, The RTT Collaborative David Schmitz MD, Associate Director for Research and Development)
Rural Residencies are the Top Predictor of Future Rural Practice
Increasing rural programs for training residents from both rural and urban backgrounds, as well as recruiting more rural students to medical education, could increase the number of rural family physicians.
Patterson DG, Shipman SA, Pollack SW, et al. Growing a rural family physician workforce: The contributions of rural background and rural place of residency training. Health Serv Res. 2023; 1-7. doi:10.1111/1475-6773.14168